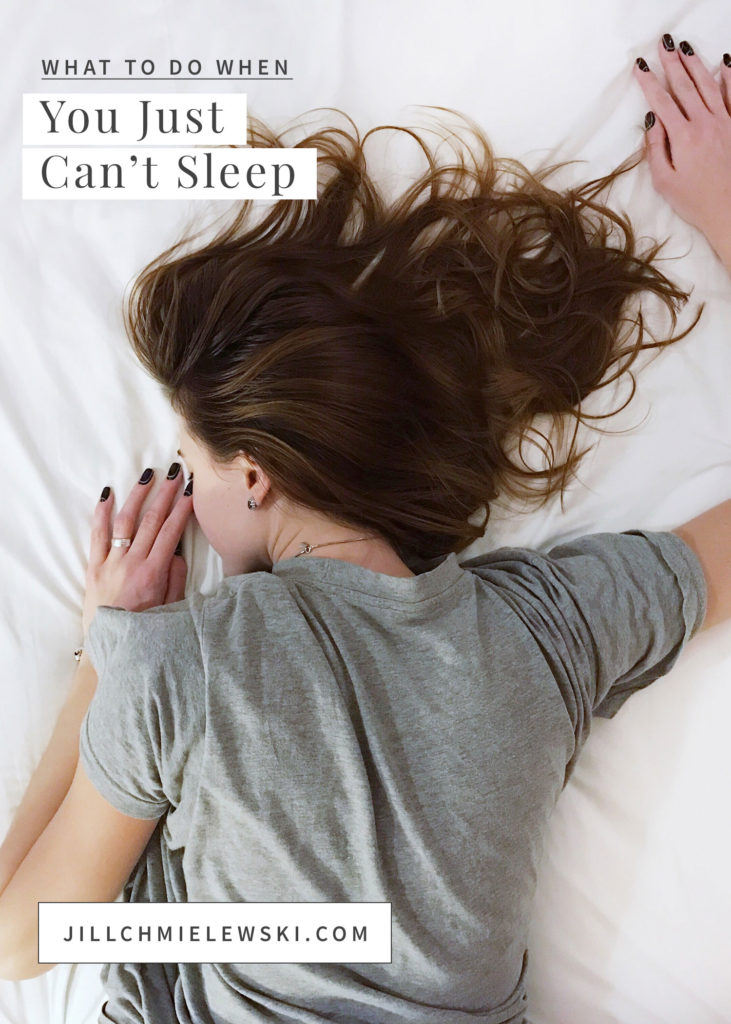
Chances are if you’re in your peri-menopausal or menopausal years, you’ve had your fair share of sleepless nights. I know I have. And most of my clients have too.
It’s a common problem among us midlife mommas, so much so, that a good number of my clients and girlfriends tell me that they have just learned to live with it. No matter what they do, they can’t seem to sleep, so they may as well accept this as their ‘new normal.’
If you’re one of those gals who isn’t sleeping well, you’re in good company. More than 30% of us have trouble sleeping. But just because sleep issues are common, doesn’t mean that they are normal. With a little bit of sleep know-how, along with some targeted sleep support remedies, you’ll be getting uninterrupted sleep in no time.
Let me start off by saying that we need sleep.
We cannot be healthy without adequate sleep. PERIOD. The vast majority of women report that they wake up most mornings feeling tired. The medical community estimates that insomnia is the #1 health-related problem in America.
Why?
Because sleep is when our body does its critical repair work, and without restorative sleep, ALL of our body’s systems suffer.
We are the health of our cells, and cellular repair happens when we sleep. We make hormones, neurotransmitters, and anti-inflammatory substances when we sleep. Our bods clean up the metabolic waste from the day when we sleep.
We can eat a perfect diet and take all the right supplements, but if we are not sleeping well, our bod is not going to function well.
Sleep is so vital that without it, we run the risk of developing a whole laundry list of physical issues, including:
- MEMORY AND COGNITIVE PROBLEMS
- WEAKENED IMMUNE SYSTEM
- MOOD CHANGES AND ANXIETY
- DECREASED PHYSICAL AND EMOTIONAL RESILIENCE
- DECREASED ABILITY TO HANDLE STRESS
- WEIGHT GAIN AND INCREASED CRAVINGS
- POOR HORMONE FUNCTION
- POOR DIGESTION
- POOR REPRODUCTION
- INCREASED AGING
- SKIN PROBLEMS
- CHRONIC INFLAMMATION
- WORSENING INSULIN RESISTANCE and;
- INCREASED RISK FOR OBESITY, TYPE 2 DIABETES & CARDIOVASCULAR DISEASE
Why are so many of us having sleep issues?
We are living as modern-day superwomen.
We’re putting the pedal to the metal, rushing and racing through our days. The stress of daily life leads to a chronic elevation in stress hormones, which mucks with our other hormones and causes HPA (hypothalamus-pituitary-adrenal) dysregulation.
Translation? Let’s just say that our hormonal systems are out of whack~ our bods release stress hormones at night before bed when they should be producing melatonin, our sleep hormone. We end up lying awake at night, feeling tired yet wired.
Our diet certainly doesn’t help matters.
We often start our day with caffeine and a sugary muffin, bagel or granola bar, and we continue this sugar-laden, caffeinated diet until we hit the sheets at night. Sugar and caffeine are stimulating to our bods, and pumping our bods full of them during the day certainly isn’t going to create the stage for a restful and calming night’s sleep. Am I right?
Many of us don’t have adequate levels of melatonin.
As the sun begins to set, melatonin, our primary sleep hormone gradually begins to rise. This is the hormone that helps us fall asleep and STAY asleep.
The hormone melatonin is made from serotonin. The bulk of serotonin is made in our gut. If we suffer from gut issues, including leaky gut, or our gut microbiome is imbalanced, we can wind up with inadequate levels of serotonin, which in turn means our bods won’t be able to make melatonin.
Melatonin has an antagonistic relationship with serotonin. It may be helpful to picture melatonin and serotonin as a seesaw. When one goes up, the other goes down, and vice versa. These hormones are guided by our internal 24-hour biological clock called the circadian rhythm, which naturally boosts serotonin during the day and melatonin at night.
We expose our eyes to too much artificial light and blue light, and not enough daylight.
The blue light from our TVs and electronic devices halts the production of melatonin, our sleep hormone. Since most of us spend our evening watching TV or combing through our electronic devices, we are pretty much guaranteed a crappy night’s sleep. If you absolutely must expose your eyes to blue light at night, then do yourself a favor and grab yourself a pair of blue light blocking glasses or clips to help block out the blue light.
Peri-menopausal and menopausal hormone changes impact our sleep.
Progesterone, in particular, is our calming hormone. Since progesterone levels begin to drop in our mid to late 30’s, we tend to experience an increase in sleepless nights as we age. Low levels of estrogen and testosterone can cause insomnia and affect our bladder health, causing frequent trips to the bathroom at night, which can prevent us from getting a good night’s sleep.
So, what can we do for a better night’s sleep?
Let’s start with some of the basics that, when done consistently can have a HUGE impact on sleep.
1. Cut out the processed foods.
Sugar-laden nutrient-devoid foods do nothing to support our hormones or our brain health, and they tend to wreak havoc on our gut health as well. Replacing them with a more nutrient-dense diet will go a long way toward promoting a good night’s sleep.
2. Limit your caffeine intake, and avoid caffeine after 10 am.
Some of us are very slow caffeine metabolizers ~ meaning we break caffeine down slowly. So that after-lunch coffee or mid-afternoon piece of dark chocolate that may not seem to be a problem is likely still in your system when you are trying to hit the sheets at night.
3. Limit your fluid intake before bed.
While I am a big fan of staying hydrated, too many fluids before bed means lots of trips to the bathroom. Try to drink the bulk of your fluids earlier in the day.
4. Reduce your exposure to artificial light.
It only takes one tiny pulse of light to disrupt our natural serotonin- melatonin seesaw,
so do your best to avoid artificial light exposure within two hours before going to bed. Ideally, you would turn off your digital devices at night, but we know that is not always feasible. At the very least, turn your digital devices’ “Night Shift” setting on, so that your digital device screen reduces its blue light emissions.
5. Use blackout shades on your windows to make your bedroom dark.
We want to do our best to tune into our body’s natural internal circadian rhythm. A bright room tells our body that it is time to wake-up, which is the opposite of what we want our bods to-do to come nightfall. A darkened bedroom signals to your body that it is time to go to sleep (and stay asleep). You might consider a sleep mask to help you out on this one.
6. Cover your digital device.
If you are using a digital alarm clock, or your phone as an alarm clock, toss a towel over the face of the clock/phone or better yet, plug it in away from your bed (we put ours in the master bathroom). Your body will thank you.
7. Go to bed when you are tired.
If you push past your natural sleep cues to get one more thing done, you often end up with a second wind, making it difficult to fall asleep. Pushing yourself to get one more thing done is NEVER worth it in the end! It’s important to listen to your body and hit the sheets when your body starts to signal that it is getting tired.
8. Don’t go to bed with a full stomach, BUT don’t go to bed starving either.
Some people sleep better if they have a little something in their tummy, especially those with digestive issues or those with a tendency for hypoglycemia (low blood sugar). But most of us tend to toss and turn if we go to bed with a full belly. Eating dinner earlier in the night can make all the difference.
9. Create a relaxing, sleep-inducing bedroom.
Soft cozy bedding in soothing colors, wooden bed frames, romantic artwork, and photographs that you love can be game-changers for a comfy bedroom. Dropping the temp in your bedroom just slightly before hitting the sheets can be helpful too. Most people sleep better and find a deeper sleep when they sleep in a cool room.
10. Set a bedtime routine.
Most of us run around like a chicken with our head cut off all day and then wonder why we can’t fall right to sleep as soon as our head hits the pillow.
If our nervous system has been in overdrive for 16 hours, it’s unrealistic to assume that it can switch into low gear in a matter of minutes simply because we want it to. It may sound like a “baby-toddler” thing to do, but remember the days when you set a bedtime routine for your child? A lavender bath, rocking in a chair, maybe a bedtime story? You too can benefit from some type of bedtime routine. Routines help your body to understand what is coming next. Consider perhaps a warm bath with essential oils or an epsom salt bath, a quiet meditation, a brief journal entry, or some gentle yoga poses to help wind down before bed.
11. Set a waking routine.
A morning routine can be just as powerful as a bedtime routine. Remember how melatonin rises as the sun goes down? Well, melatonin quickly plummets when the retina of our eyes is exposed to light, and as a result, our serotonin surges. So, waking up, pulling the curtains back, and looking out at the morning sun will naturally tell your body to wake up and get ready for the day. When we slowly wake, slowly wander out of bed, we don’t experience that same serotonin surge, and we tend to feel sluggish throughout the morning.
Remember, we are trying to live in alignment with our body’s natural cues. It may be helpful to think about life before electricity. Our ancestors rose with the sun and slept when the sun went down. While it may not be realistic to hit the sheets when the sun goes down, it’s important to start living (and sleeping) according to our body’s natural biological design, rather than forcing our bodies to push beyond their natural limits.
12. Go to bed earlier.
The bulk of our deep, restorative sleep naturally occurs between the hours of 11 pm and 3 am, so getting to bed well before midnight allows your body to do its important repair work critical for healthy cell function and healing.
13. Cut back on the booze.
Alcohol tends to interrupt our rapid eye movement (REM) sleep, the part of our sleep cycle when we are in major repair mode. I get it…. alcohol helps you to fall asleep, but for most of us, especially when we have multiple drinks, our body pays the price.
14. Check your mattress.
People tend to keep their beds for far too long, so pay attention to whether the mattress itself may be to blame for a poor night’s sleep. You can’t expect to have a good night’s sleep lying on a lumpy, lopsided mattress.
If you have honestly tried all of the above and the quality of your sleep has not budged, then perhaps your brain isn’t able to make enough melatonin to ensure uninterrupted sleep all night long, or there is a chemical imbalance preventing sufficient relaxation.
You might consider a few targeted sleep remedies:
1. For peri-menopausal and menopausal sleep issues
Replacing lost estrogen, progesterone, and testosterone can be very helpful for women in the peri-menopausal and menopausal years. Estrogen deficiency causes sleep maintenance insomnia, which means waking at 2 or 3 am. Progesterone is good for sleep because it converts to a sedating neurosteroid called allopregnanolone or ALLO which soothes the GABA receptors in the brain (GABA is our calming neurotransmitter). Low testosterone can cause bladder issues as well as insomnia, so having adequate hormone levels can help us get a good night’s rest.
If hot flashes are an issue, cutting back on alcohol and caffeine can make a big difference.
I often recommend that my clients suffering from hot flashes/night sweats incorporate two tablespoons of flaxseeds into their daily routine. Flaxseeds contain weak plant estrogens that can prevent erratic estrogen fluctuations (the cause of hot flashes). Always buy organic flaxseeds in their whole seed form, and grind them at home in a coffee grinder, storing them in the refrigerator to prevent them from becoming rancid.
Valerian may help insomnia during perimenopause. Valerian has been used medicinally since the times of early Greece and Rome to treat sleeplessness, nervousness, trembling, headaches, and heart palpitations. A study from 2011 showed Valerian improved the quality of sleep in women with menopause who suffered from insomnia. And unlike sleeping aids that can cause grogginess in the morning, Valerian does not appear to affect alertness or concentration the next morning. Valerian can take up to one month to see a noticeable benefit, but it may be worth considering if you suffer from sleeplessness due to low estrogen. Follow the manufacturer’s instructions for dosing.
2. For trouble winding down at night or trouble falling asleep
Remember earlier when I mentioned that high nighttime cortisol (the stress hormone) can cause sleep issues? The combination of Ashwagandha AND Magnesium Glycinate in the evening can often help reduce cortisol levels and relax the bod.
If you are not falling asleep because of low melatonin production at bedtime, you might consider a melatonin supplement. I always recommend starting low around 0.5 mg or so 30 minutes before bedtime, and increasing as needed. Taking too much melatonin will result in grogginess the next morning. This is best for short-term use only, as using it long term can potentially halt your body’s internal production of melatonin.
3. For trouble staying asleep
If you are waking up in the middle of the night, it might be because you have an insufficient continuous supply of melatonin throughout the night, in which case melatonin isn’t going to help.
Remember earlier when I said that the body makes melatonin from serotonin? Well, we make serotonin from an amino acid called 5-HTP (5-hydroxytryptophan). Instead of taking melatonin before bed, you can actually take a 5-HTP supplement. Once taken, the body will convert 5-HTP to serotonin within just a few hours, which should help to ensure a steady and continuous supply of melatonin to get you through the night.
Warning: Keep in mind that 5-HTP is contraindicated if you take any SSRI or SNRI (or other serotonin-enhancing) antidepressant or sleep medications such as Zoloft, Trazadone, Wellbutrin, Ambien or you may end up with a toxic surplus of serotonin.
4. If you have a racing mind
Remember earlier when I mentioned the calming neurotransmitter GABA? Well, its counterpart is glutamate, which is considered an excitatory neurotransmitter. For various reasons, some women have too much glutamate at night when they should have GABA. Ashwagandha or Holy Basil before bed can be helpful (along with magnesium). The amino acid NAC (N-acetyl cysteine) suppresses the brain’s synthesis of glutamate and promotes conversion to GABA. I have personally found that taking NAC before bed can work wonders to calm my racing mind.
Two other amino acids ~ L-theanine and Taurine have been shown to have a calming effect on the brain. L-theanine is an amino acid found in green tea and Taurine is an amino acid that reduces cortisol levels and increases the production of GABA, which is a major inhibitory neurotransmitter—our bodies’ natural “off” switch.
Metagenics makes a formula called ‘Trancor’ the includes several of the remedies listed above. I’ve included several of the sleep remedies listed here under the “Favorites” heading on Fullscript. You can check those out by clicking here.
As always, be sure to check with your physician or licensed health care practitioner before trying any new supplements.
Happy sleeping!